Did you know that obesity goes beyond just affecting your weight? It can significantly impact your risk of developing diabetes.
Understanding the mechanisms behind this relationship is crucial for effective prevention and management. From insulin resistance to hormonal changes, the ways in which obesity contributes to diabetes risk are multifaceted and complex.
By exploring these four key pathways, you'll gain valuable insights into how excess weight can influence your likelihood of developing diabetes.
Key Takeaways
- Obesity leads to insulin resistance, increasing diabetes risk.
- Excess adipose tissue triggers inflammation, impairing insulin function.
- Visceral fat release harmful substances affecting metabolic function.
- Hormonal imbalance from obesity promotes insulin resistance and diabetes development.
Insulin Resistance and Obesity

When obesity is present, it often leads to insulin resistance, a key factor in the development of diabetes. Research findings have shown that the excess adipose tissue in obese individuals releases inflammatory markers, which interfere with the normal function of insulin, resulting in insulin resistance.
To manage obesity-related insulin resistance effectively, it's crucial to focus on weight loss through a combination of dietary modifications and regular physical activity. Studies have demonstrated that even a modest weight reduction of 5-10% can significantly improve insulin sensitivity and reduce the risk of developing diabetes in obese individuals.
Furthermore, incorporating whole foods rich in fiber, lean proteins, and healthy fats into your diet can aid in weight management and improve insulin sensitivity. Regular exercise, such as aerobic activities and strength training, has been proven to enhance insulin action and promote weight loss.
Inflammatory Response and Weight Gain
Excess adipose tissue in obese individuals triggers an inflammatory response that plays a significant role in the progression of weight gain and metabolic dysfunction. This inflammatory response is characterized by the release of various inflammation markers from the adipose tissue, such as cytokines like tumor necrosis factor-alpha (TNF-alpha) and interleukin-6 (IL-6). These markers can disrupt the normal functioning of insulin, leading to insulin resistance and impaired glucose metabolism.
As the adipose tissue expands in obesity, it undergoes changes that promote the infiltration of immune cells, further exacerbating the inflammatory state. This chronic low-grade inflammation not only contributes to weight gain but also sets the stage for the development of metabolic diseases like type 2 diabetes.
Furthermore, the inflammatory response can interfere with adipose tissue's ability to properly store and release fatty acids, leading to ectopic fat deposition in organs like the liver and muscles, which further impairs insulin sensitivity. By understanding the intricate relationship between inflammation and adipose tissue, strategies can be developed to target these pathways and potentially mitigate the risk of diabetes associated with obesity.
Impact of Visceral Fat on Diabetes
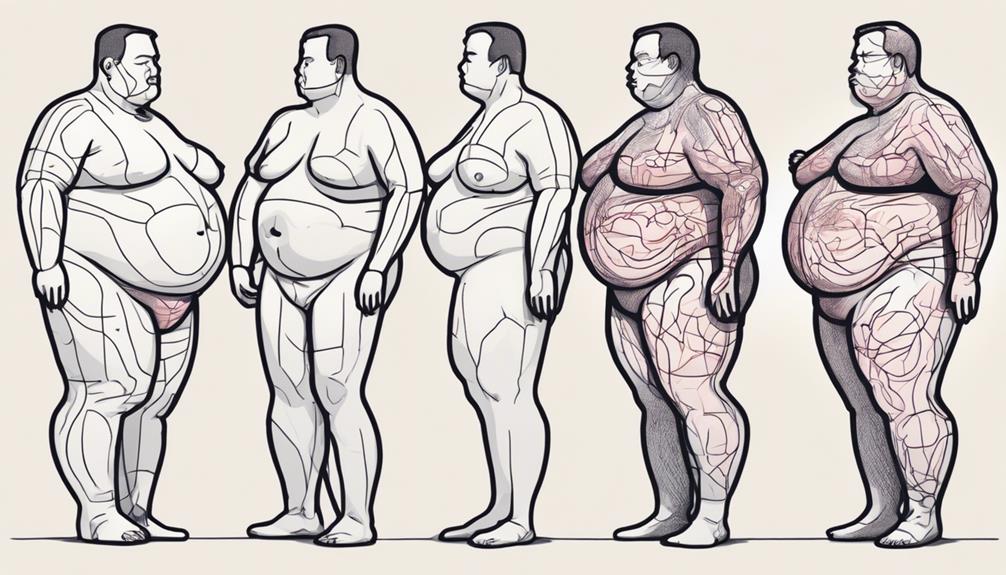
The accumulation of visceral fat in individuals with obesity significantly contributes to the development and progression of diabetes through intricate metabolic interactions and inflammatory processes. Visceral fat, specifically located around organs in the abdominal cavity, plays a crucial role in increasing diabetes risk.
Here are some key points to consider:
- Visceral fat is metabolically active, releasing harmful substances that can lead to insulin resistance.
- This type of fat affects the liver's ability to regulate blood sugar levels, promoting hyperglycemia.
- Inflammatory molecules produced by visceral fat can impair pancreatic function, disrupting insulin production.
- Excessive visceral fat can alter adipokine secretion, contributing to chronic low-grade inflammation associated with diabetes.
- The close proximity of visceral fat to vital organs makes it a significant factor in promoting systemic metabolic dysfunction and insulin sensitivity.
Understanding how visceral fat impacts diabetes risk highlights the importance of managing weight distribution to reduce the likelihood of developing diabetes.
Obesity-induced Hormonal Changes
Obesity-induced hormonal changes intricately influence metabolic pathways, further exacerbating the risk of developing diabetes by disrupting essential endocrine functions. Hormonal imbalance effects play a crucial role in the link between obesity and diabetes. Adipose tissue, particularly visceral fat, secretes various hormones and cytokines that modulate insulin sensitivity and glucose metabolism. In obesity, these adipokines become dysregulated, promoting insulin resistance and inflammation, key drivers of type 2 diabetes.
Leptin and adiponectin are adipokines that regulate appetite and energy balance. In obesity, leptin resistance can develop, leading to increased food intake and decreased energy expenditure. Adiponectin levels decrease in obesity, contributing to insulin resistance and a pro-inflammatory state. Additionally, obesity-related metabolic changes, such as elevated free fatty acids, further disrupt insulin signaling pathways, impairing glucose uptake in muscle and fat cells.
Understanding the intricate interplay of hormonal changes induced by obesity is crucial in comprehending the pathophysiology of diabetes. Addressing these hormonal imbalances through lifestyle modifications and medical interventions is essential in managing and preventing diabetes in individuals with obesity.
Frequently Asked Questions
How Does Genetics Play a Role in the Relationship Between Obesity and Diabetes Risk?
Genetic predisposition can influence how obesity impacts your diabetes risk. Gene-environment interaction plays a crucial role in metabolic health. Understanding your genetic makeup can help tailor interventions to mitigate diabetes risk associated with obesity.
Can Losing Weight Help Reverse Insulin Resistance in Individuals With Obesity?
Losing weight can greatly improve insulin sensitivity in individuals with obesity. This can lead to a reversal of diabetes risk factors. By shedding excess pounds, you can positively impact your body's ability to regulate blood sugar levels and reduce diabetes risk.
Are There Specific Dietary Changes That Can Help Reduce Inflammation in the Body and Lower Diabetes Risk?
Making smart dietary changes can significantly reduce inflammation and lower your diabetes risk. By incorporating anti-inflammatory foods like leafy greens, berries, and fatty fish into your meals, you can support your overall health.
What Role Do Sleep Patterns and Stress Levels Play in the Impact of Visceral Fat on Diabetes Risk?
To understand the impact of visceral fat on diabetes risk, consider your sleep quality and stress levels. Research links poor sleep and high stress to increased visceral fat, which can elevate diabetes risk. Prioritize rest and stress management for better health.
Are There Any Specific Exercises or Lifestyle Changes That Can Help Regulate Hormonal Imbalances Caused by Obesity?
To regulate hormonal imbalances caused by obesity, consider making lifestyle modifications. Engage in regular physical activity, prioritize balanced nutrition, and aim for quality sleep. These changes can contribute to hormonal regulation and overall well-being.
Conclusion
Just as a storm gathers strength from the heat of the sun, obesity fuels the fire of diabetes risk through various pathways.
Insulin resistance acts as the lightning, striking at the body's ability to regulate blood sugar.
Inflammation serves as the thunder, rumbling with the weight gain caused by excess fat.
Visceral fat looms like dark clouds, casting a shadow over metabolic health.
Hormonal changes swirl like gusts of wind, disrupting the delicate balance within the body.